When your Autoimmune Disease Looks Like Depression
Many people with an autoimmune disease like Sjogren’s had symptoms for a long time before discovering the explanation. Very often, patients will emphasize fatigue and pain when describing symptoms to their doctors. After all, those two things have a HUGE impact on quality of life.
What do those two symptoms often point to?
Raise your hand if you received a diagnosis of depression, but thought “I don’t think that’s what it is”.
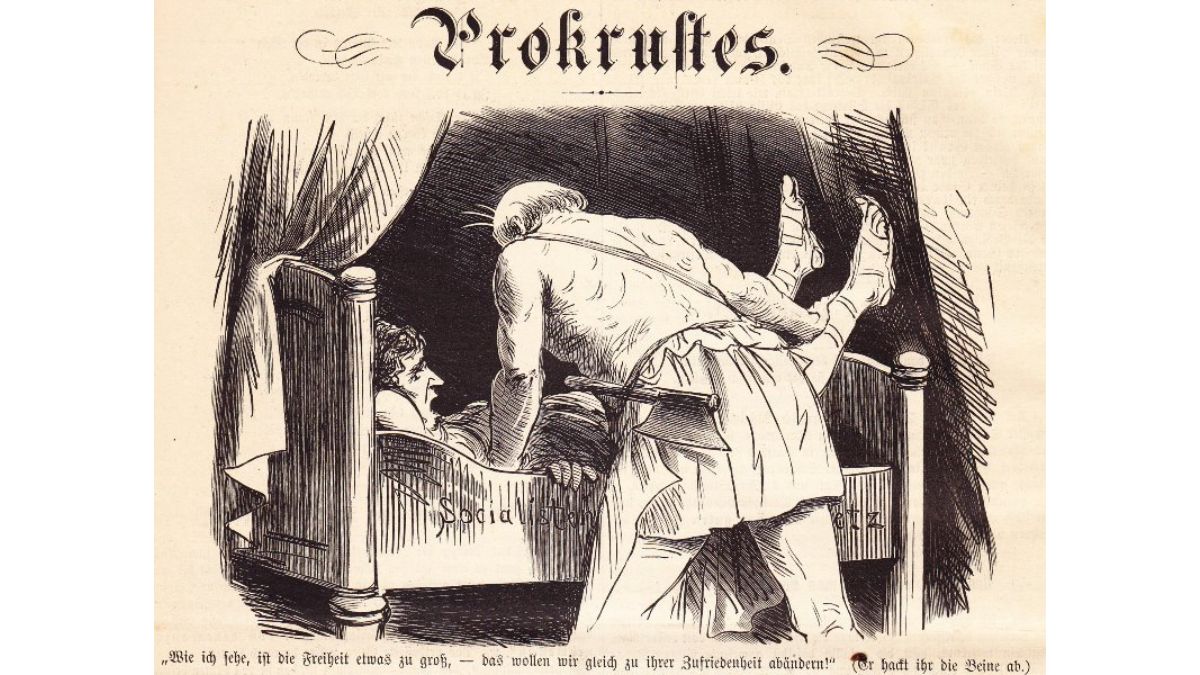
Now let me tell you about a Greek Mythological figure called Procrustes.
A “Procrustean Bed” is known as a concept, theory, or diagnosis that becomes the “go-to” explanation when there are no obvious answers otherwise. You’ll find this happening in many facets of life, but in medicine, many doctors have one of these, and that bed is often called “depression”. You have chronic fatigue and pain? There’s no medical reason I can find? Let me treat (or refer) you for depression.
Don’t get me wrong, it is GREAT that awareness and acceptance of depression has grown in recent years. After all, there is nothing to be ashamed of when you are truly clinically depressed. However, it’s best for clinicians to always take a step back and see if there is another explanation for what people are feeling and experiencing.
Now, doctors, I’m not accusing you of doing anything nefarious at all. We ALL DO IT in one way or another in life. We all view the world, or our work, in this case, from a certain perspective that has been correct at some point. In this case, however, all the emphasis on catching and addressing mental health diagnoses, while very well-intended, has its own drawbacks.
Squeezing the Balloon
I remember very clearly when I was in clinical psychology practice in a medical facility, the resident physician and I would joke about “squeezing the balloon” back and forth.
He would refer someone to me that had symptoms of depression (often with very good reason, I might add) and say the physical symptoms they reported were psychosomatic. In other words, depression and stress were manifesting physically and they just needed a psychologist, not a medical doctor.
So he squeezed his side of the metaphorical balloon, and the bulge of air in the balloon went toward me. With some of these patients, I would say “it’s more than that, please check again”. Then I would squeeze my side of the balloon, and the bulge of air went back to him. Back and forth it would go.
Autoimmune Disease and Depression
Now that I’ve said all that, I don’t want to give the impression that a diagnosis of depression is never warranted. It most certainly is for some. For starters, people with mental health diagnoses related to severe stress and trauma are at increased risk of autoimmune disorders.
A new diagnosis that isn’t going away can feel like a gut punch. The limitations that come with autoimmune diseases very often make it difficult to live the life you want. Fatigue gets in the way of doing the things you love. Financial strain from managing the conditions is enough to bring anyone down. People not understanding you can lead to conflicts and feeling isolated. So clearly, autoimmune disease and depression often coexist.
Of course, treat the depression. But keep in mind that it’s one part of a larger clinical picture. It’s best to work to get everything else under control while you manage the mood symptoms, and don’t assume that resolving psychological problems will magically fix the medical.
It’s a two-way street: while mood symptoms can manifest physically, illness can really bring a person down. It’s in a patient’s best interest to recognize this and treat the patient accordingly.